Introduction:
Autologous stem-cell transplantation (ASCT) remains an integral part of therapy for many newly diagnosed and relapsed multiple myeloma (MM) patients. Most tertiary centers rely on age, ECOG status, and multi-organ function evaluation to determine eligibility for ASCT. African Americans (AA) have a higher incidence of monoclonal gammopathy of undetermined significance (MGUS), higher incidence of MM and higher mortality rates than their Caucasian counterparts, mainly due to lower access to care. Furthermore, AA patients are also underrepresented in clinical trials. Studies have shown AA patients have similar to improved progression-free survival (PFS) and overall survival (OS) compared to Caucasian patients when similar therapies are offered to both groups; however, lower rates of transplantation are reported among AA patients. This is likely multifactorial in origin, with varying risk factors, biological influences, and social hindrances leading to racial disparity. We sought to examine the differences in rates of ASCT among African Americans vs Caucasian patients.
Methods:
We conducted a retrospective chart review of all patients with myeloma referred to our center between 2018 and 2022. Information regarding demographics, referral information, insurance and transplant status obtained for all patients referred and/or transplanted at our center were obtained from this chart review. The diagnosis date was obtained from referral records if they were referred from an outside institution. All patients received therapy at the discretion of treating physicians. Statistics are descriptive.
Results:
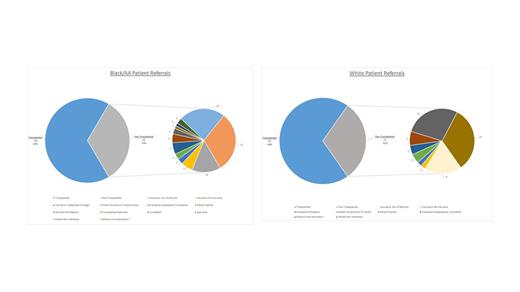
206 AA patients were referred to our center for transplant evaluation, of which 138 underwent autologous transplantation (67%). Additionally, 141 Caucasian patients were referred to us for transplant evaluation, 98 of which underwent ASCT (69%). The transplant rates were similar across both genders among AA patients, with female AA patients accounting for 49% of all AA transplants. Among Caucasian patients, female patients accounted for 37% of all Caucasian transplants. The median referral delay time was 104 days among AA patients and 85 days among Caucasian patients. The median time from the date of referral to transplant was 128 days for AA patients and 124 days for Caucasian patients. The reasons for non-transplant varied between the two races. For African Americans, the most common reason was medical contraindication followed by patient disinterest in contrast to Caucasian patients, which was patient disinterest followed by medical contraindication.
Conclusion: Once referred to a tertiary center, we observed no racial disparities among transplants in AA and Caucasian patients. While the median time from the date of referral to the date of transplant was similar across both groups, we noted an increased referral delay among AA patients.
Disclosures
Keruakous:Janssen: Consultancy, Membership on an entity's Board of Directors or advisory committees, Research Funding; BMS: Membership on an entity's Board of Directors or advisory committees. Cortes:Biopath Holdings: Consultancy, Current holder of stock options in a privately-held company, Membership on an entity's Board of Directors or advisory committees, Research Funding; Abbvie: Consultancy, Research Funding; Forma Therapuetic: Consultancy; Gilead: Consultancy; Takeda: Consultancy, Honoraria; Novartis: Consultancy, Research Funding; Pfizer: Consultancy, Research Funding. Kota:Pfizer: Honoraria; Kite: Honoraria; Novartis: Honoraria; Incyte: Research Funding.